Abstract
Previous research demonstrated that patients with hematologic malignancies have a high probability receiving intensive care at their end-of-life (EOL). In this study, we assessed EOL quality measures in patients with hematologic malignancies before and after starting the provision of a specialist palliative care service.
We conducted a retrospective cohort study in Komaki City Hospital. Provision of the specialist palliative care service was started in our hospital on April 1, 2012. We reviewed the medical records of all adult patients who died of hematologic malignancies between April 1, 2007 and March 31, 2017. Patients who had been cared for in the Departments of Hematology and Palliative Care were included. This study was approved by the institutional review board of Komaki City Hospital. We assessed the prevalence and trends of multiple measures of intensive EOL care established in the peer-reviewed literature. Intensive EOL care was defined as the occurrence of at least one of the following acts: 1) cardiopulmonary resuscitation (CPR) in the last 30 days of life, 2) intubation in the last 30 days of life, 3) intensive care unit (ICU) admission in the last 30 days of life, 4) chemotherapy use within the last 14 days of life, 5) receiving red cell transfusions within the 7 days before death, and 6) receiving platelet transfusion within the 7 days before death. Analysis of frequencies was performed using Fisher's exact test for 2 x 2 tables. The Cochran-Armitage test was used to test for trends over time.
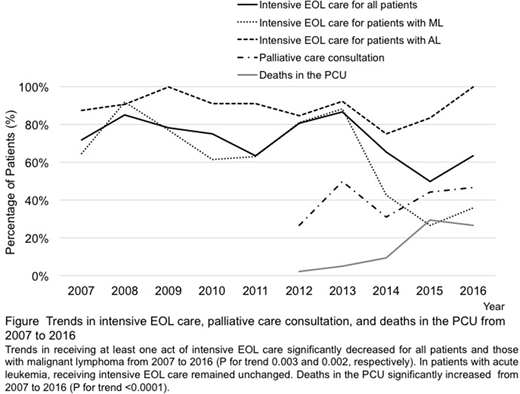
A total of 351 consecutive patients who died from hematologic malignancies were identified: 176 before and 175 after April 1, 2012. The median age at death was 73 years old. These included 150 patients with non-Hodgkin lymphoma, 113 with acute myeloid leukemia, 63 with multiple myeloma, 11 with acute lymphoblastic leukemia, 8 with chronic lymphocytic leukemia, and 5 with Hodgkin lymphoma. A total of 69 (39%) received specialist palliative care consultation and 24 (14%) died in the palliative care unit (PCU) after April 2012. Deaths in the PCU increased from 1 (2%) in 2012 to 8 (27%) in 2016 (P for trend <0.001). The median time from palliative care referral to death was 26 days (interquartile range [IQR]: 10-49 days). The length of stay in the PCU was 16 days (IQR: 9.5-22.5 days).
Cases of CPR in the last 30 days of life decreased from 4 (13%) in 2007 to 0 in 2016 (P for trend <0.001). Intubations in the last 30 days of life also decreased from 2 (6%) in 2007 to 1 (3%) in 2016 (P for trend 0.046). Platelet transfusions within 7 days before death decreased from 18 (56%) in 2007 to 14 (47%) in 2016 (P for trend 0.031). There were no significant decreases in ICU admissions in the last 30 days of life, chemotherapy use within the last 14 days of life, or receiving red cell transfusions within 7 days before death from 2007 to 2016. Patients receiving at least one act of intensive EOL care significantly decreased from 23 (72%) in 2007 to 19 (63%) in 2016 (P for trend 0.019).
Compared with patients with acute leukemia (AL), those with malignant lymphoma (ML) were more likely to receive specialist palliative care consultation (49% vs. 27%, respectively; P=0.010) and die in the PCU (21% vs. 5%, respectively; P=0.007). In patients with ML, deaths in the PCU increased from 1 (5%) in 2012 to 7 (50%) in 2016 (P for trend <0.001).
In patients with ML, cases of chemotherapy use within the last 14 days of life decreased from 5 (22%) in 2007 to 2 (14%) in 2016 (P for trend 0.030). Patients with ML who received palliative care consultation were less likely to receive platelet transfusion within 7 days before death compared with those who did not (28% vs. 51%, respectively; P=0.041). In patients with ML, those receiving at least one act of intensive EOL care significantly decreased from 11 (65%) in 2007 to 5 (35%) in 2016 (P for trend <0.001). In patients with AL, there was no significant difference in chemotherapy use within the last 14 days of life or receiving transfusions within 7 days before death between patients who received specialist palliative care and those who did not. All patients with AL received at least one act of intensive EOL care in 2016.
These findings suggest that specialist palliative care improved the quality of EOL care in patients with hematologic malignancies, especially in those with ML. However, in patients with AL, EOL care is still suboptimal with the provision of specialist palliative care.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal